Welcome to Jiangsu Yigao Medical
Welcome to Jiangsu Yigao Medical
 E-MAIL:[email protected]
E-MAIL:[email protected]

Electric operation tables have become an indispensable tool in modern surgical settings, providing a range of benefits that enhance both the precision and efficiency of surgical procedures. These advanced tables, equipped with intelligent electric systems and pull-cord control mechanisms, play a critical role in improving the overall surgical experience for both the medical staff and patients. Below are some of the key ways in which electric operation tables contribute to enhanced surgical precision and efficiency:
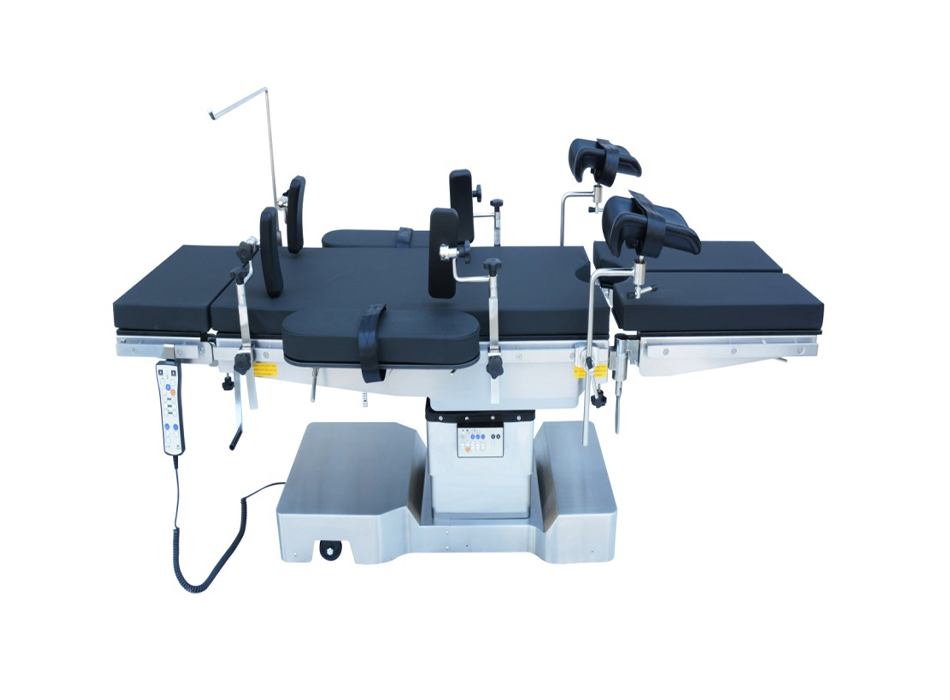
Electric operation tables are indispensable tools in modern operating rooms, offering the ability to provide highly accurate and customizable positioning that is critical for surgical precision. These tables feature a sophisticated motor system that allows seamless adjustments in various parts of the table. This precision not only enhances the safety and comfort of the patient but also plays a crucial role in improving the efficiency of the surgical team. In this section, we will explore the key adjustable components of electric operation tables, including height adjustments, tilt adjustments, and backboard and legboard positioning.
Electric operation tables are engineered to cater to a wide range of surgical specialties, offering specific functions and fine-tuned positioning adjustments that ensure optimal access to surgical sites. By providing surgeons with easy, precise control over these features, the tables reduce the need for manual repositioning and enable rapid adjustments even in the most sterile environments.
One of the most fundamental adjustments in electric operation tables is the ability to modify the height. This adjustment has a profound impact on the ergonomics and comfort of the surgical team. Surgeons often work long hours in challenging positions, and if the operating table is not properly adjusted, they may experience fatigue, strain, or discomfort. The high-performance motors in electric operation tables allow for smooth and precise height adjustments, ensuring that the table is positioned at the optimal level for the surgeon’s work.
For many surgeons, maintaining proper posture during surgery is essential to prevent long-term musculoskeletal issues. An electric operation table that allows precise height adjustments can significantly improve the surgeon’s comfort and reduce physical strain. Whether the surgeon is performing a delicate procedure on a patient lying flat or in a more upright position, the ability to adjust the height ensures that they can maintain an ergonomic stance, which is particularly beneficial during lengthy operations.
Height adjustments are not only important for ergonomics but also for surgical flexibility. During surgeries, there may be moments when the surgeon needs to alter their position or shift focus between different areas of the patient’s body. With an electric system, height changes can be made seamlessly with minimal disruption to the procedure. Surgeons can adjust the table height without relying on manual effort, making it easier to reposition the patient without causing delays or compromising the sterility of the environment.
In addition to benefiting the medical staff, height adjustments also ensure that patients are positioned correctly for their surgeries. Whether it’s to maintain alignment during spinal surgery or to accommodate certain anatomical positions in gynecological procedures, having the ability to fine-tune the table height ensures that patients are safe, stable, and as comfortable as possible throughout the procedure.
The ability to adjust the tilt of the operating table is another critical feature of electric operation tables. Surgeons often require access to different angles of a patient’s body during surgery, and tilt adjustments can make this process much easier. Electric operation tables allow for precise adjustments to the front and rear tilt, as well as side tilt, giving surgeons the ability to fine-tune the table’s positioning based on the surgical site.
For many procedures, particularly in abdominal, thoracic, or orthopedic surgeries, the ability to tilt the table forward or backward can provide the surgeon with better access to the target area. For example, tilting the table can help reposition the patient’s body to improve visibility and surgical access in the abdominal cavity, or assist in positioning the patient’s head and neck during spinal surgeries.
In complex surgeries, where a clear line of sight and proper body positioning are critical, the front and rear tilt adjustments allow surgeons to achieve a precise angle without having to move the patient or change their posture. This flexibility ensures that the surgical site remains optimally exposed, even as the surgery progresses through different stages.
In addition to front and rear tilt, side tilt is another crucial adjustment feature. The side tilt provides the ability to adjust the patient’s lateral position, allowing the surgical team to gain better access to specific surgical sites. This feature is especially useful in procedures such as urological surgery, where the surgeon needs to position the patient’s body in such a way that allows for clear access to the target organ.
Side tilt adjustments are also essential in emergency surgeries, where quick positioning changes are necessary to address life-threatening conditions. The ease and precision of electric controls allow medical staff to adjust the table to the optimal tilt with minimal disruption to the ongoing procedure.
The ability to make precise tilt adjustments during surgery directly impacts the outcome of the procedure. Surgeons can better manage patient positioning, ensuring that the surgical area is exposed to the right degree, and minimizing the time spent re-positioning the patient. This can significantly shorten the overall duration of the surgery, reducing anesthesia time and minimizing potential complications.
Electric operation tables come with highly customizable backboard and legboard positioning. These components are particularly important in certain types of surgery, such as orthopedic, gynecological, and spinal surgeries, where precise positioning of the patient’s back and limbs is crucial for achieving optimal surgical outcomes.
The backboard is an essential component of electric operation tables that helps position the patient’s upper body. In spinal surgeries, precise backboard adjustments are crucial to ensure that the spine is aligned properly and that the surgeon has full access to the surgical area. By adjusting the backboard, surgeons can raise or lower the patient’s torso, tilt it at specific angles, and maintain optimal access to the spine or surrounding structures.
In orthopedic surgeries, backboard positioning helps maintain the alignment of the patient’s body during joint surgeries. For example, knee and hip surgeries require the surgeon to position the patient’s legs in a certain way to ensure proper access to the surgical site. An electric operation table allows for fine-tuning of these adjustments, ensuring that the procedure can be performed with maximum accuracy.
The ability to adjust the legboard is particularly important in lower limb surgeries, such as hip replacements or orthopedic trauma procedures. By positioning the legboard to accommodate the patient’s legs in the correct position, the surgeon gains the necessary access to the hip, knee, or other joints without having to make additional adjustments during the procedure.
Electric operation tables allow for precise legboard adjustments, ensuring that the patient’s legs are properly aligned and supported throughout the surgery. This reduces the need for manual repositioning, ensuring that the procedure is efficient and that the patient’s comfort and safety are maintained.
Electric operation tables allow surgical teams to make quick, accurate adjustments without compromising the sterility of the environment or interrupting the procedure. In high-pressure surgeries, where time is critical and precision is essential, these tables help streamline the entire surgical process. Surgeons can make adjustments with the push of a button or a pull of a cord, enabling faster reactions to any unexpected changes or needs during surgery.
Electric operation tables are designed to cater to a wide variety of surgical specialties, each with unique requirements. Here’s a quick comparison of how table adjustments support different types of surgeries:
| Surgical Specialty | Adjustments Needed | Why They Matter |
|---|---|---|
| Orthopedic Surgery | Backboard and legboard positioning, tilt adjustments | Proper limb alignment and optimal exposure to joints |
| Gynecological Surgery | Height adjustments, tilt adjustments, backboard positioning | Clear access to the pelvic area and precise alignment |
| Spinal Surgery | Backboard positioning, height adjustments | Ensures proper spine alignment and optimal surgical access |
| Abdominal Surgery | Tilt adjustments, height adjustments | Access to the abdominal cavity with optimal patient positioning |
| Urological Surgery | Side tilt adjustments, height adjustments | Allows for optimal positioning to access the urinary system |
The operating table is far more than a simple platform for a patient to lie on during a procedure. In contemporary surgical practice, it is the central, functional hub around which the entire operation revolves. Its positioning, stability, and configurability directly influence the surgeon's ability to perform with precision, the anesthesiologist's capacity to manage the patient's physiology, and the scrub team's efficiency in assisting. Any disruption or inefficiency related to the table can create ripples of delay and increased risk throughout the operative environment. Therefore, the evolution from mechanical, manually-cranked tables to advanced electric operation tables represents a quantum leap in optimizing the surgical workflow. These sophisticated systems are engineered not just for patient positioning, but to actively enhance the procedural rhythm, minimize non-surgical tasks, and uphold the stringent demands of asepsis.
Surgical workflow is a complex, time-sensitive sequence of events where every second counts. Efficiency is not about rushing; it is about eliminating unnecessary motions, reducing cognitive load, and ensuring that tools and equipment are responsive to the dynamic needs of the surgery. Inefficiencies often manifest as:
- Time Delays: Manual adjustment of a table requiring multiple personnel and physical effort.
- Break in Sterility: A team member needing to touch a non-sterile surface to adjust the table, requiring a change of gloves and pausing the procedure.
- Surgeon Distraction: The lead surgeon having to verbally direct a complex repositioning, diverting focus from the critical anatomy.
Electric operation tables are specifically designed to mitigate these inefficiencies at their source.
The core of the improved workflow lies in the intuitive design of the control systems. These interfaces are the point of interaction between the human intent of the surgical team and the electromechanical response of the table.
The most significant innovation for workflow is the ubiquitous pull-cord control pendant. This handheld unit, often sheathed in a sterile plastic cover, is the primary tool for intraoperative adjustments. Its design philosophy is rooted in ergonomics and asepsis:
- Sterile Accessibility: The pendant is easily held by the sterile scrub nurse or surgeon, allowing them to make adjustments directly without calling for assistance from non-sterile circulating staff.
- Ergonomic Button Layout: Controls are logically grouped and often color-coded or icon-based for instant recognition—a green button for Trendelenburg, a blue one for reverse Trendelenburg, arrows for height, etc. This minimizes the need for looking away from the surgical field.
- Precision Movement: Buttons allow for smooth, incremental, and quiet adjustments, enabling fine-tuning of the patient's position by millimeters or degrees to achieve the perfect surgical view.
Beyond manual control, advanced tables feature memory functions that store pre-programmed positions for common procedures. With a single button press, the table can automatically reconfigure itself into a standard position for a laparoscopic cholecystectomy, a lateral decubitus for hip replacement, or a beach-chair for shoulder arthroscopy. This eliminates the time-consuming and potentially error-prone process of manually setting each segment (back section, leg section, tilt) at the beginning of a case.
| Control Feature | Workflow Impact | Benefit to Sterility |
| Sterile Pull-Cord Pendant | Enables immediate adjustments by sterile team members, eliminating verbal requests and wait times. | Allows sterile team to operate the table without breaking the aseptic field. |
| Pre-programmed Positions | Reduces table setup time from minutes to seconds at the start of and during procedures. | Minimizes the number of touches and adjustments required, reducing potential contamination points. |
| Fine Motor Control | Allows for ultra-precise positioning, optimizing the surgical view and reducing surgeon fatigue. | Prevents the need for large, disruptive movements that could jeopardize sterile drapes. |
| Remote Control (Non-sterile) | Allows circulating nurses to assist with major repositioning without entering the sterile core. | Maintains a clear separation between sterile and non-sterile personnel. |
The physical and cognitive burden of operating a manual table is non-trivial. Cranking handles requires strength, time, and coordination between staff. This physical effort is entirely eliminated with electric tables. The "minimization of manual effort" has a twofold positive impact:
1. Physical Conservation: The nursing and tech staff are spared physically demanding work, reducing their fatigue over long operating days. This contributes to a safer environment and better staff retention.
2. Cognitive Conservation: The surgeon is liberated from the mental load of orchestrating table movements. Instead of thinking, "I need the table up 2 cm and tilted left 5 degrees, who can do that?" they can simply request, "Please adjust for a better angle," and the scrub nurse executes it instantly. This preserves the surgeon's cognitive resources for decision-making related to the procedure itself, such as anatomical dissection, implant placement, or managing unexpected bleeding.
The workflow advantages are perhaps most pronounced when considering the immutable rules of the sterile field. The operating table, being large and essential, is a major potential vector for contamination. It is covered in sterile drapes, but its controls are fundamentally non-sterile. The traditional model required a non-sterile circulator to be called over, the surgeon or nurse to verbally explain the needed adjustment, and the circulator to manually input the change on a non-sterile control panel. This process is slow and introduces a risk of miscommunication.
The electric table with a sterile pull-cord control shatters this inefficient model. It effectively creates a "sterile bridge" to the table's functionality. The sterile team member, with their gloved hand on the sterile-covered pendant, becomes the direct operator. This maintains the integrity of the sterile field, reduces verbal clutter and potential miscommunication in the OR, and speeds up the entire process. The team can respond to the surgeon's needs in real-time, as fluidly as passing a new instrument.
The improvement to surgical workflow provided by electric operation tables is holistic. It is not a single feature but the synergistic combination of intuitive control, pre-programmed automation, ergonomic design, and unwavering support for aseptic technique that creates the benefit. By streamlining the non-surgical, logistical tasks of patient positioning, these tables allow the entire team—surgeons, anesthesiologists, nurses, and technologists—to function at their highest level. The focus narrows and sharpens on the patient and the procedure, leading to smoother operations, reduced operative times, and an environment where precision and safety are paramount. This technological advancement is a foundational element of the modern, high-performance operating room.
In the high-stakes environment of an operating room, patient safety is the unwavering cardinal rule. Every piece of equipment, from the smallest scalpel to the largest imaging machine, is scrutinized for its potential to cause harm. The operating table, as the primary patient interface, carries an immense safety responsibility. It must be an unyielding pillar of stability, a secure platform that actively protects the patient from inadvertent injury. The transition from hydraulic or mechanical manual tables to advanced electric motor systems represents a profound evolution in fulfilling this safety imperative. These systems are engineered not merely for convenience but to provide a fundamentally safer foundation for surgical care, mitigating risks that were once inherent in surgical positioning.
The core of the enhanced safety profile lies in the sophisticated electric motor and control system. Unlike manual systems that may rely on hydraulic fluid (which can leak or compress) or mechanical cranks with potential for slippage, electric systems provide direct, digitally-controlled actuation.
Electric motors drive each table function—height adjustment, tilt, Trendelenburg, and segment articulation (back, leg, etc.)—through precision gear systems. This design eliminates the "play" or slight give often found in mechanical systems. When a position is set, the motors effectively lock the table into place with a degree of rigidity that is difficult to achieve manually. The power is not just for movement but for maintaining an immutable position, even under significant load or when forces are applied during surgery.
The risk in manual adjustment often lies in the movement itself. A sudden release of a hydraulic valve or an over-enthusiastic turn of a crank can lead to jarring, sudden shifts. Electric motors, in contrast, enable smooth, gradual, and controlled movement. The speed of adjustment is regulated and consistent, preventing any rapid or unexpected motions that could startle the surgical team, disrupt the surgical field, or, most critically, injure the patient. This smoothness is paramount when positioning patients with spinal injuries or critical vascular access.
| Safety Feature | Mechanism of Action | Patient Benefit |
| Precision Electric Locking | Digital motors and gears lock table segments into position with zero backlash or slippage. | Eliminates risk of unintended movement during critical stages of surgery, ensuring a stable operative field. |
| Gradual Power-Assisted Movement | Motors provide smooth, controlled, and slow adjustment at the push of a button. | Prevents jerky movements that could lead to soft tissue strain, nerve stretch, or disruption of vital lines/tubes. |
| High Weight Capacity & Low Center of Gravity | Robust chassis and motor design ensure stability even at maximum height and with heavy patients. | Virtually eliminates the risk of table tipping, enhancing safety for bariatric and all patient populations. |
| Fail-Safe Braking Systems | Redundant electronic and mechanical brakes engage automatically in case of power failure. | Guarantees patient security regardless of external circumstances, providing ultimate peace of mind. |
The stability of an electric operating table directly addresses a spectrum of potential patient injuries.
This is the most fundamental safety concern. The rigid locking mechanisms and robust construction of electric tables ensure that even at extreme tilts or heights, the patient platform remains secure. The risk of a table component suddenly giving way is reduced to near zero.
Many surgical injuries are not related to the procedure itself but to prolonged or improper positioning. These include:
- Nerve Damage: Ulnar, peroneal, and brachial plexus nerves are vulnerable to compression or stretch. The smooth, incremental adjustability of electric tables allows the team to achieve the ideal position without forcing limbs into place, minimizing pressure on nerves.
- Pressure Ulcers: Long procedures can lead to tissue ischemia and sores. The ability to make micro-adjustments to segments easily helps redistribute pressure points throughout a long surgery.
- Orthopedic and Spinal Stability: In trauma and orthopedic surgeries, the patient's injury itself creates vulnerability. A sudden jarring movement from a table could exacerbate a spinal fracture or disrupt a reduced fracture. The controlled motion of an electric table is essential for safe positioning in these cases.
The value of stability is magnified in procedures where millimeter precision is demanded.
In cranial or spinal procedures, the surgeon is often working with microscopic instruments around critical neural structures. Any shift in the patient's position, no matter how minute, can have catastrophic consequences. The absolute stability of an electric table, free from drift or sag, provides the confidence required for such meticulous work. Furthermore, the fine control allows for precise adjustments to the head clamp or spinal alignment without disturbing the entire patient.
Systems like the da Vinci Surgical System are mounted to the operating table. Any movement or vibration in the table is transferred directly to the robotic arms, magnifying the effect and potentially causing dangerous movements at the surgical site. The rock-solid foundation provided by a high-quality electric operating table is a prerequisite for safe robotic surgery, ensuring the robotic platform remains perfectly stable throughout the operation.
During laparoscopic procedures, the surgeon operates through fixed trocars inserted into the abdominal wall. If the table is moved after trocar placement, the relationship between the instruments and the internal anatomy changes, which can strain port sites, increase the risk of internal injury, and complicate the dissection. The precise and predictable movement of an electric table allows the entire team to be repositioned as a single unit if needed, maintaining the crucial fixed geometry of the ports.
True safety engineering anticipates failure. Premium electric operation tables incorporate multiple layers of protection:
- Backup Power Systems: Internal batteries ensure the table remains operational and can be adjusted even during a main power failure.
- Manual Overrides: In the exceedingly rare event of a complete motor failure, mechanical manual release systems are in place to allow for manual cranking, ensuring the patient is never stranded in an unsafe position.
- Error Detection: Modern tables have self-diagnostic systems that can detect motor overload or system faults, alerting the staff to potential issues before they become critical.
The modern operating room (OR) is a symphony of advanced technology, where the harmonious interplay between various devices is paramount to surgical success, patient safety, and operational efficiency. At the heart of this technologically advanced ecosystem lies the electric operating table. Far from being a passive platform, it has evolved into a dynamic, intelligent hub that facilitates seamless integration with a wide array of surgical equipment and instruments. This integration is a critical component in the development of the "connected OR," minimizing disruptions, streamlining workflows, and ultimately creating a highly coordinated environment tailored to the precise demands of each surgical procedure.
The concept of the connected OR revolves around the interoperability of all its components. In this setup, the electric operating table acts as a central command post, communicating with and controlling other devices either through wired connections or, increasingly, via secure wireless protocols. This central role transforms the table from a mere piece of furniture into an active participant in the surgical process.
One of the most crucial integrations is with surgical visualization equipment, namely overhead surgical lights and high-definition monitors. This synergy is vital for providing the surgical team with an unobstructed and perfectly illuminated view of the operative field.
Surgical Lights: Modern electric tables can communicate directly with robotic or manual surgical lights. When the table is repositioned—for example, tilted into a Trendelenburg position—the integrated system can automatically adjust the focus and trajectory of the surgical light to maintain optimal illumination on the now-angled surgical site. This eliminates the constant manual readjustment of lights by nurses or surgical assistants, which can be a significant source of frustration and delay during critical moments. The system ensures that the light follows the field, not the fixed position of the table.
Medical Monitors: Similarly, monitors displaying vital signs, endoscopic camera feeds, ultrasound imaging, or navigation data are often mounted on booms around the OR. Through integration, the positioning of these monitors can be linked to the table's configuration. As the table height or angle changes, the monitors can automatically adjust their height and swivel to maintain the perfect line of sight for the surgeon and the entire team. This prevents neck strain, reduces the need for verbal commands to adjust screens, and ensures that critical data is always readily visible without any obstructions.
Beyond visualization, the electric operating table's adaptability is fundamental to organizing the physical space for instruments and personnel. Its ability to achieve a vast range of positions directly creates a more ergonomic and efficient workspace.
Creating the Instrument Landscape: Complex surgeries, particularly in fields like orthopedics, cardiothoracic, and neurology, require a plethora of specialized instruments. The configuration of the table directly influences how these instruments are arranged and accessed. For instance, a table that can be lowered significantly allows for easier placement of large C-arms for intraoperative fluoroscopy without compromising the sterility of the field. The ability to create a "bridge" or "lateral bend" can physically make room for instrument trays, robotic arms, or other large equipment to be positioned closer to the patient, reducing the reach required by the scrub nurse.
Reducing "Search Time": In a non-integrated, disorganized environment, a significant amount of time can be lost to "searching"—whether for the right instrument or for a better view. A seamlessly integrated table mitigates this. By pre-programming positions for specific phases of a surgery (e.g., "initial incision," "cardiac bypass," "closure"), the table, lights, and monitors all move in concert to a pre-defined configuration that is known to be optimal. This pre-planning ensures that instrument tables are within easy reach, visualization is perfect, and the team does not need to pause to physically hunt for tools or readjust equipment. This fluidity maintains the surgical rhythm and can tangibly reduce operative time.
The following table illustrates common surgical specialties and how specific table integrations directly enhance the procedure:
| Surgical Specialty | Common Table Position | Integrated Equipment | Benefit of Integration |
| Orthopedics (Spine) | Wilson Frame, Reverse Trendelenburg | C-arm, Surgical Navigation System | Table communicates with navigation for perfect patient registration; low profile allows C-arm to rotate 360° for unobstructed AP/lateral views. |
| Laparoscopy | Steep Trendelenburg | Monitor Booms, Insufflator | Monitors auto-tilt to remain in surgeon's sightline as table angles; table securely holds patient in position to prevent sliding. |
| Robotic Surgery | Lithotomy, Low Lithotomy | Robotic Console, Robotic Arms | Precise, remote-controlled micro-adjustments of the table can be made without disturbing docked robotic arms, fine-tuning the operative field. |
| Neurology | Fowler's Position, Head Elevated | Surgical Microscope | Table interfaces with microscope; if the surgeon repositions the microscope, the table can make fine adjustments to follow, keeping the target centered. |
The next frontier of integration moves beyond physical coordination into the realm of data. The most advanced electric operating tables are equipped with sensors and software that can feed valuable information into the OR's central network.
These tables can monitor their own status—including height, tilt, and segment positions—and relay this data in real-time. This information can be used for:
Patient Safety: The system can be integrated with patient warming devices. If the table is raised significantly, increasing the distance between the patient and a forced-air warmer, the warmer can automatically increase its output to compensate and maintain normothermia.
Documentation and Billing: Specific table attachments and positions used for a procedure can be automatically logged into the patient's electronic health record (EHR) and even facilitate more accurate billing for the specialized equipment utilized.
Preventive Maintenance: The table can self-diagnose and report its maintenance needs to hospital engineering teams, predicting failures before they occur and ensuring maximum uptime.
For this seamless integration to be universally achievable, the adoption of standardized communication protocols like ORi™ (Operating Room Interface) is essential. These protocols act as a common language, allowing equipment from different manufacturers to communicate effectively with each other and with the hospital's information systems. This breaks down proprietary barriers and allows hospitals to build a truly best-in-class, integrated OR environment without being locked into a single vendor.
The physical well-being of the surgical team is a critical, yet often overlooked, component of a successful operating room (OR). Long, complex procedures demand immense mental concentration and physical stamina from surgeons, anesthesiologists, nurses, and technicians. Historically, the manual adjustment of heavy, mechanical operating tables was a significant source of unnecessary physical strain, contributing to staff fatigue and even long-term musculoskeletal injuries. The advent of electric operation tables has revolutionized this dynamic, transforming a physically taxing chore into an effortless, precision task. By eliminating manual effort, these advanced tables play a pivotal role in preserving the energy and focus of the entire medical team, thereby directly enhancing both staff welfare and patient safety.
The traditional operating room presents a unique set of ergonomic challenges. Surgical teams often maintain static, awkward postures for hours, performing repetitive, fine motor tasks. The manual adjustment of an old-fashioned table compound these issues dramatically. These adjustments are not merely inconvenient; they represent a genuine occupational hazard.
Manual tables require significant brute force to manipulate. Cranking handles, pumping foot pedals, and releasing heavy mechanical locks are actions that engage large muscle groups and can lead to acute strain.
High Force Exertion: Moving a table segment—such as raising the back section or tilting the entire table—with a patient on it requires considerable physical strength. This is not a one-time event; repositioning may be required numerous times throughout a single surgery to optimize access or respond to the surgical phase.
Awkward Postures and Repetitive Motions: The cranks and levers are often poorly positioned from an ergonomic perspective. A nurse or technician might have to bend, twist, or kneel to reach them, putting stress on the back, shoulders, and wrists. Repeating these motions over weeks, months, and years is a primary contributor to work-related musculoskeletal disorders (MSDs).
Unexpected Resistance and Injury Risk: Older mechanisms can jam or provide unexpected resistance, leading to a sudden, jarring movement that can cause acute muscle pulls or strains. The simple act of adjusting the table becomes a moment of potential injury, distracting the team from the patient on the table.
The physical strain is accompanied by a significant cognitive and workflow disruption. The process of manually adjusting a table is rarely swift or silent.
Breaking Concentration: A surgeon deeply focused on a delicate dissection must pause and wait for the table to be adjusted. The sounds of cranking and the physical movement can break the rhythm and concentration of the entire team.
Inefficiency and Delays: The process requires a staff member to disengage from their primary role (e.g., a scrub nurse moving away from the instrument table) to perform a manual labor task. This introduces delays and creates a disjointed workflow, potentially prolonging the time the patient is under anesthesia.
Electric operation tables address these challenges comprehensively by transferring the physical burden of adjustment from human muscle to electric motors. This is achieved through intuitive control systems, often featuring handheld pendants or touchscreen interfaces that allow for precise, silent, and effortless positioning.
The core benefit of electric tables lies in their profound positive impact on ergonomics and staff health.
Elimination of Forceful Exertion: Adjusting the table now requires only the gentle press of a button. There is no cranking, no pumping, and no straining. This removes a major risk factor for MSDs, helping to protect the careers of OR staff and improve their long-term quality of life.
Promotion of Neutral Postures: The handheld remote control can be operated from a comfortable, neutral standing or sitting position. Staff no longer need to contort their bodies to reach awkwardly placed mechanical controls. This promotes better posture throughout the surgical procedure.
Reduced Fatigue: By conserving the physical energy that would have been wasted on manual adjustments, the entire team experiences less overall fatigue. This is especially crucial during marathon surgeries that can last many hours. A less fatigued team is sharper, more alert, and capable of maintaining a higher level of performance from the first incision to the final suture.
The advantages extend far beyond mere physical comfort, deeply influencing the cognitive and procedural aspects of surgery.
Uninterrupted Focus: Adjustments become instantaneous and nearly silent. The surgeon can request a change in table height or tilt and have it executed immediately without a pause in the procedure. This maintains the "surgical flow state," a period of intense concentration and peak performance that is crucial for complex operations.
Empowerment and Efficiency: Control is decentralized and can be given to the most appropriate team member. Often, the surgeon themselves holds a pendant, allowing them to make micro-adjustments without verbal commands. Alternatively, the circulating nurse can make adjustments without leaving their station. This streamlines communication and improves overall OR efficiency.
Precision Positioning: Electric controls allow for incredibly fine, millimeter-scale adjustments. This level of precision is impossible to achieve with manual force and is often critical for perfecting the surgical view or aligning a patient for a specific technique, such as in orthopedic or spinal procedures.
The following table contrasts the key aspects of manual versus electric operation tables from the perspective of staff strain and OR efficiency:
| Aspect | Manual Operation Tables | Electric Operation Tables |
| Physical Effort Required | High force exertion; repetitive cranking/pumping | Minimal; single button press |
| Risk of Musculoskeletal Injury | High; significant risk of acute and chronic strain | Very Low; ergonomic controls eliminate forceful exertion |
| Speed of Adjustment | Slow and labor-intensive | Rapid and immediate |
| Noise Level | Audible cranking and clanking | Near-silent operation |
| Surgical Flow Disruption | High; breaks concentration and rhythm | Low; seamless and integrated into procedure |
| Precision of Positioning | Coarse; difficult to make fine adjustments | Highly precise; programmable, micro-adjustments possible |
Investing in electric operation tables is, fundamentally, an investment in human capital. The reduction of physical strain has a direct and positive cascade effect on the entire OR environment.
The physical toll of OR work is a contributing factor to staff burnout and turnover. By creating a safer, less physically demanding work environment, hospitals can improve job satisfaction, reduce absenteeism due to injury, and retain experienced, valuable staff. A team that feels its well-being is valued is a more cohesive and motivated team.
Ultimately, any factor that affects the surgical team affects the patient. A fatigued, distracted, or physically strained surgeon or nurse is more prone to error. By minimizing physical strain and fatigue, electric tables help ensure that the medical team is operating at their full cognitive and physical capacity. This heightened state of alertness directly translates to enhanced vigilance, better decision-making, and a higher standard of patient care and safety throughout the surgical procedure.
The modern healthcare institution is a complex ecosystem comprising numerous surgical specialties, each with its own unique set of procedural requirements, patient positioning needs, and equipment integration demands. In this diverse environment, the operating table is far more than a passive surface; it is a fundamental piece of surgical technology that can either enable or hinder a procedure. Electric operation tables have emerged as the cornerstone of the versatile operating room, precisely because of their unparalleled flexibility. This inherent adaptability allows a single table platform to be configured and reconfigured to meet the exacting demands of a vast spectrum of surgical specialties, from general surgery to complex orthopedics and neurology. This multi-functionality transforms the electric table from a specialized tool into a cost-effective, universal asset for hospitals and clinics, ensuring high levels of precision, efficiency, and safety across the entire surgical services department.
The design philosophy behind advanced electric operation tables is to create a universal platform that serves as a stable, reliable, and highly adaptable foundation for any surgical intervention. This is achieved through a combination of modular design, extensive articulation, and programmable functionality. Unlike specialty-specific tables of the past, which might be optimized for one discipline but useless in another, the modern electric table is a master of all trades. Its value lies in its ability to be perfectly tailored for each trade with minimal effort and time.
The flexibility of electric tables is rooted in two key engineering principles: modularity and articulation.
Modular Design: These tables are designed with a system of interchangeable accessories and components. The core table top is often a rigid, radiolucent carbon fiber base to which various sections and attachments can be added. For example:
- A split-leg section can be attached for lithotomy positioning in gynecological or urological procedures.
- A removeable headrest section allows for the attachment of specialized neurosurgical or cranial fixation headsets.
- Extension plates can be added to accommodate taller patients, a common need in orthopedic trauma surgery.
- Arm boards, leg holders, and shoulder supports are all swappable components that allow for the precise limb positioning required in specialties like orthopedics or plastic surgery.
Extensive Articulation: Electric motors drive the movement of individual table segments with high precision. A typical multi-segment table can independently control the:
- Back section (Trendelenburg, reverse Trendelenburg, Fowler's position)
- Leg section (flexion, extension, lowering)
- Table height (from very low for ergonomic surgeon seating to very high for open procedures)
- Lateral tilt (left and right roll)
- Overall table tilt
This range of motion allows the table to achieve hundreds of possible configurations, each ideal for a different surgical access point and anatomical focus.
The true test of an electric table's flexibility is its performance across the broad spectrum of surgical specialties. Its ability to adapt is what makes it indispensable.
The following table outlines how a single, well-designed electric operation table meets the specific needs of various medical fields:
| Surgical Specialty | Critical Positioning Needs | How Electric Tables Deliver |
| General & Laparoscopic Surgery | Steep Trendelenburg for pelvic access; reverse Trendelenburg for upper abdomen; secure patient positioning to prevent sliding. | Precise motorized tilt to exact angles; contoured padding and safety straps; low height setting to accommodate surgeon ergonomics during long procedures. |
| Orthopedics & Spine | Full radiolucency for imaging; fracture table attachments; ability to position for lateral, prone, and supine approaches; extreme stability. | Carbon fiber top for unobstructed X-rays; modular attachments for traction; powerful motors to hold heavy patients securely in complex poses like lateral decubitus. |
| Urology & Gynecology | Lithotomy position for perineal access; easy access for C-arm for endourology; kidney bridge position for renal surgery. | Quick-attachment lithotomy stirrups; ability to flex the table to create a "kidney bridge"; central break in table top for instrumentation. |
| Cardiothoracic & Neurology | Reverse Trendelenburg for cranial procedures; lateral positioning for thoracic access; precise head fixation; compatibility with microscopes and navigation. | Fine-adjustment controls for micro-positioning of the head; interfaces for Mayfield skull clamps; stable base for robotic and navigation systems. |
| Bariatric Surgery | Exceptional weight capacity; extra-wide table top; reinforced structure to ensure safety. | Engineered to hold patients over 500kg; wide modular tops and accessories; high-power motors for safe and smooth positioning. |
For hospital administrators and OR managers, the flexibility of electric operation tables translates directly into a compelling financial argument. The multi-specialty capability of a single table model offers significant economic advantages over maintaining a fleet of older, specialty-specific tables.
Reduced Need for Multiple Tables: Instead of purchasing and maintaining a dedicated orthopedic table, a dedicated laparoscopy table, and a dedicated urology table, a hospital can outfit multiple ORs with the same model of flexible electric table. This standardization means that any OR can be rapidly configured for any type of surgery scheduled that day, dramatically increasing room utilization efficiency.
Simplified Inventory and Training: Standardizing on a flexible table platform simplifies the management of accessories and spare parts. It also streamlines staff training, as surgeons, nurses, and technicians only need to become proficient on one system rather than several different ones. This reduces errors and improves setup speed.
Future-Proofing the Investment: Medical technology and surgical techniques evolve rapidly. A table that is only suitable for today's procedures may become obsolete tomorrow. A highly flexible electric table, however, can adapt to new techniques, new technologies (like advanced robotics), and new procedural demands, protecting the capital investment for a much longer period.
The adaptability of these tables provides OR schedulers with unprecedented flexibility. An operating room is no longer "the orthopedic room" or "the gynecology room"; it is simply "an operating room." This allows for more dynamic and efficient scheduling, reducing downtime between cases. The quick and easy reconfiguration of the table means turnover time is minimized. A team can finish a laparoscopic cholecystectomy, quickly change the accessories and set a new patient position, and be ready for a podiatry case in a fraction of the time it would take to move a patient to a completely different, specialized table in another room.
Ultimately, the goal of this flexibility is not merely convenience or cost savings—it is to improve surgical outcomes. The ability to achieve and maintain the perfect position for every procedure is a critical factor in surgical success. It provides the surgeon with optimal access and visualization, reduces tissue strain, and minimizes the risk of patient injury related to positioning (e.g., nerve damage, pressure ulcers). The precision of electric adjustments ensures this position is achieved accurately and reproducibly every time. The efficiency gains from quick setup and changeover contribute to reduced anesthesia time for the patient, which is directly linked to better postoperative recovery.